Over the past two decades, we have had significant shifts in the number and effectiveness of opioid policies at state and federal levels.(1) This includes access to Prescription Drug Monitoring Programs (PDMPs), access to naloxone, limits on prescribing, and required referral to pain specialists, among others.(1) Opioid dispensing rates peaked at 2012 at 81.3 prescriptions per 100 persons. Due to a variety of factors, the nation saw opioid dispensing rates fall to a low of 43.3 prescriptions per 100 persons, the lowest rate in the past 15 years, though some counties had levels nine times that.(2)
In 2016, the Centers for Disease Control (CDC) issued guidelines for the use of opioids in the treatment of chronic non-cancer pain, also colloquially known as the “CDC Guidelines”. However, these guidelines did not give recommendations for the treatment of chronic pain, but rather simply created lines in the sand for primary care physicians prescribing opioids in their clinic. In fact, no level I recommendations appeared in these guidelines, and the only level II recommendation was that patients suspected of opioid use disorder be referred for treatment. (3)
Despite the contraction and increased selectivity of opioid prescribing, the nation saw a rise in overdose death rates involving opioids over the past 20 years. This was not fueled by a change in the overdose rates associated with commonly prescribed opioids, or even heroin. Rather, it has been fueled by illicit synthetic opioids, primarily in the form of fentanyl.(4)
The principle of non-maleficence is core to the bioethics taught to our physicians as a component of the Hippocratic Oath. Primum non nocere is the principle of doing no harm, to guide physicians and patients along the pathway to shared decisionmaking regarding the risks, benefits, and alternatives to any treatment. This includes opioids, steroids, biologic agents, chemotherapy, surgery, and more. The 2016 CDC Guidelines for primary care physicians, made some specific recommendations for specific clinicians. However, these guidelines were grossly misapplied by a variety of stakeholders, including pharmacists, insurers, health systems, physicians, and more. The American Medical Association House of Delegates called out the misapplication of the 2016 Guidelines in 2018 formally as House Resolution 235. The misapplication of these guidelines was then specifically called out in 2019 (a little late) in the New England Journal of Medicine by the same authors who wrote the 2016 Guidelines. (5) Unfortunately, the 2016 Guidelines were taken up highly by pharmacies, physicians afraid of violating guidelines, and health systems with the same fear. Patient-centric opioid care was not emphasized by these guidelines, and many clinicians and clinical settings took a NIMBY (Not In My Backyard) approach to opioids, creating pain care deserts for many opioid patients.
The 2022 CDC Guidelines contains pretty specific language focusing on patient-centered decision making that occurs between the patient and their physician.(6) But much of the damage here has been done. Large numbers of patients were exposed to prescription opioids for years and years by their well-meaning physicians over the past thirty years, and this multiyear systematic abandonment of many patients did not have the intended effect of these policies, which is to save lives. What we have seen is an increase in synthetic opioid deaths, and a stigmatization of chronic pain at home, the pharmacy, the clinic, the hospital, and more.
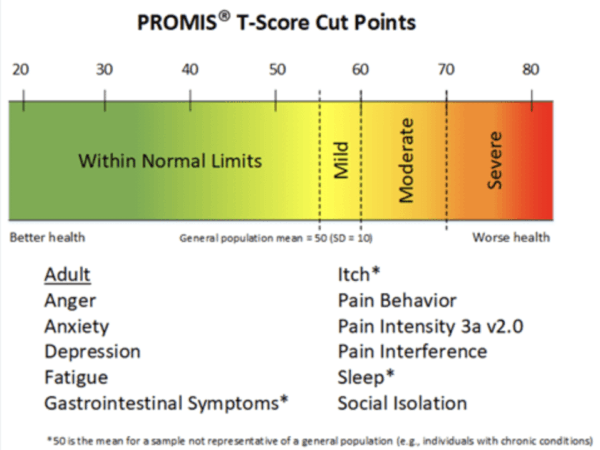
The intersection of chronic pain, opioid use disorder, social isolation, and mood disorders contains numerous intermingled variables.(7) Quantifying the contribution of these various parameters is critical to assessing risk, benefits, and alternatives in each individual patient. Opioids are not appropriate for elimination from modern medicine – they are essential medicines to a functioning society. Medical reversal is the concept that new evidence should result in a paradigm shift in care to the abandonment of a prior therapy is not rational in this instance.(8) What we really need to understand is the components of the problem, so that we can appropriately deploy solutions. This could be a variety of tailored therapies that incorporates the old (opioids, acupuncture, physical therapy, tai chi, you name it), with the new (neuromodulation, biologics, monoclonal antibodies, regenerative therapies).
Expert pain care is a discipline that is a calling to me and to many pain providers worldwide. Understanding the profile of our patients and their response to all treatments and treatment-combinations is the next step to success in this field. The next steps are not to create static guidelines, but to invest in identifying quantitative markers that can aid in the accurate and effective treatment of pain in our patients, which may require an opioid in some cases. Clinical decision support based on real world outcomes data is our best hope to informing these decisions in the future. Today, unfortunately, many of those decisions are dictated by coverage policies, not science, and surely not common sense.
1. Lee B, Zhao W, Yang KC, Ahn YY, Perry BL. Systematic Evaluation of State Policy Interventions Targeting the US Opioid Epidemic, 2007-2018. JAMA Netw Open. 2021;4(2):2007–18.
2. U.S. Opioid Dispensing Rate Maps | Drug Overdose | CDC Injury Center [Internet]. [cited 2023 Jan 4]. Available from: https://www.cdc.gov/drugoverdose/rxrate-maps/index.html
3. Dowell D, Haegerich TM, Chou R. CDC Guideline for Prescribing Opioids for Chronic Pain — United States, 2016. MMWR Recommendations and Reports [Internet]. 2016 Mar 18 [cited 2019 Jan 21];65(1):1–49. Available from: http://www.cdc.gov/mmwr/volumes/65/rr/rr6501e1.htm
4. Mattson CL, Tanz LJ, Quinn K, Kariisa M, Patel P, Davis NL. Trends and Geographic Patterns in Drug and Synthetic Opioid Overdose Deaths — United States, 2013–2019. MMWR Morb Mortal Wkly Rep. 2021;70(6):202–7.
5. Dowell D, Haegerich T, Chou R. No Shortcuts to Safer Opioid Prescribing. New England Journal of Medicine [Internet]. 2019 Apr 24 [cited 2019 Jun 7];NEJMp1904190. Available from: http://www.nejm.org/doi/10.1056/NEJMp1904190
6. Dowell D, Ragan KR, Jones CM, Baldwin GT, Chou R. CDC Clinical Practice Guideline for Prescribing Opioids for Pain – United States, 2022. MMWR Recomm Rep. 2022;71(3):1–95.
7. Sheng J, Liu S, Wang Y, Cui R, Zhang X. Review Article The Link between Depression and Chronic Pain : Neural Mechanisms in the Brain. 2017;2017.
8. Prasad V, Cifu A. Medical reversal: why we must raise the bar. Yale Journal of Biology and Medicine. 2011;84:471–8.
 According to The National Institute of Mental Health, “
According to The National Institute of Mental Health, “